A new model for clinical trials in New Zealand
A promising new cancer treatment is entering a phase 2 trial coordinated by the Malaghan Institute of Medical Research, proving New Zealand is an ideal testing ground for clinical research in CAR T-cells and other immunotherapies.
On this page
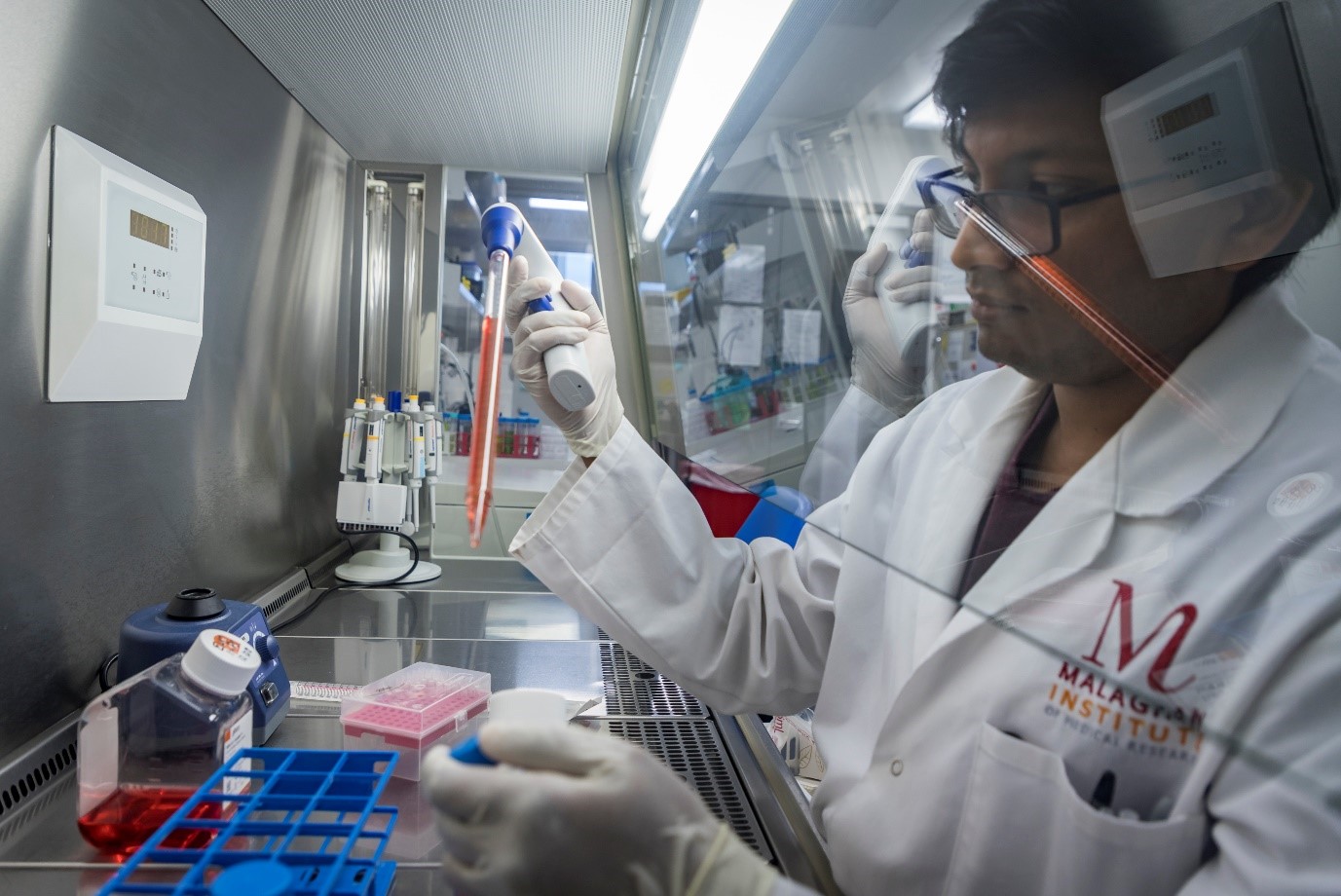
Chimeric Antigen Receptor (CAR) T-cell therapy involves redirecting a patient’s own immune cells (T-cells) to identify and attack their cancer cells. Once the personalised CAR T-cells have been made in a lab, they are administered to the patient as a one-off treatment that, if successful, has the potential to eradicate the cancer cells entirely.
“At the Malaghan Institute, we’re interested in using immune therapies to help human health. CAR T-cell therapy is the ultimate way of doing that,” says Dr Robert Weinkove, the Malaghan Institute’s Clinical Director.
“We learnt of the development of CAR T-cell treatments overseas and wanted to contribute to the global effort while addressing the health needs of New Zealanders.”
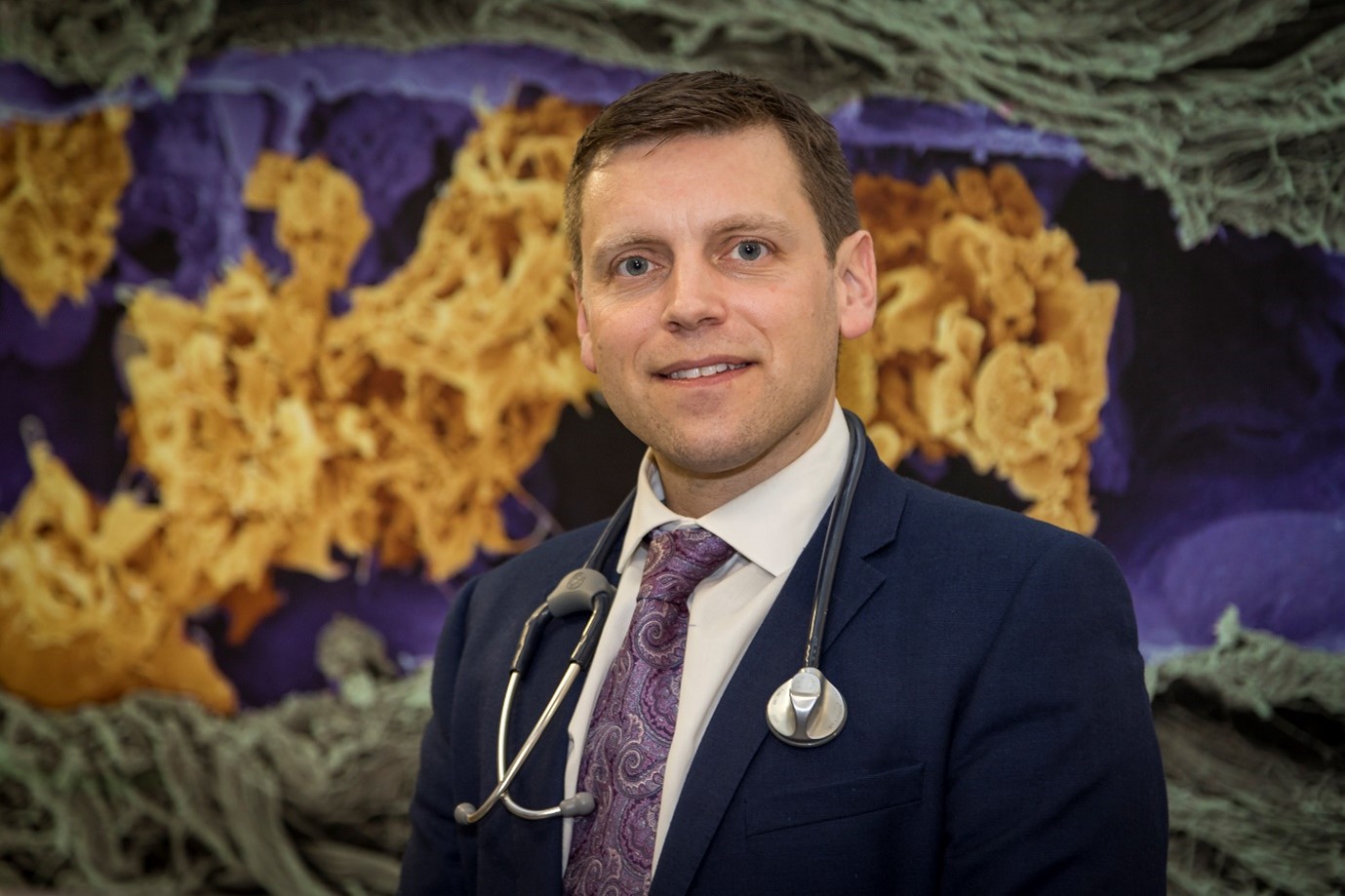
Dr Robert Weinkove, the Malaghan Institute’s Clinical Director, heads up the CAR T programme
Meeting New Zealand’s clinical needs
The Malaghan Institute was conscious of the urgent unmet clinical need in New Zealand and recognised the delays in rolling out CAR T-cell treatments here and globally due to high cost and complex logistics of personalised cellular therapies. Leveraging the institute’s experience of cellular therapy clinical trials, Dr Weinkove worked alongside colleagues including the institute’s General Manager Mike Zablocki to find innovative ways to bring CAR T-cell therapy to New Zealand.
“With collaborating researchers in Guangzhou, we had access to a new ‘third-generation’ CAR construct,” Mr Zablocki says.
“We set up Wellington Zhaotai Therapies Limited as a joint venture and we worked with them to establish a new CAR T-cell manufacturing process at the Malaghan Institute and began a phase 1 clinical trial, with parallel research to refine the original construct.”

Mike Zablocki, the Malaghan Institute’s General Manager, is focussed on the commercialisation aspects of the research.
Following the data and finding backers
The phase 1 trial, which involved 21 patients, started as a dose escalation study to establish the optimal dose level for safety and efficacy. The results showed an impressive response to the treatment at all doses but, when compared with comparable treatments overseas, suggested an improved safety profile.
While the results supported further clinical trials, the Malaghan team recognised the need to automate and scale up the CAR T-cell manufacturing procedure. To achieve this, they needed partners that were prepared to work with them to take things to the next level.
“At the time, the Government was funding the creation of technology incubators in New Zealand and there was one operated by a group called BridgeWest Ventures,” says Mr Zablocki.
“It was just one of those serendipitous things that the BridgeWest Group, a company with a history of running contract manufacturing organisations, was running a deep tech incubator here in New Zealand. We had a need and a pitch in that specific area that they understood really well, and they bought into the vision of what we were trying to do, what we were trying to create for Aotearoa.”
As a result, BioOra Limited was established, a spinout New Zealand company that specialises in automated CAR T-cell manufacture. This meant that the Malaghan Institute and others would have the ability to deliver CAR T-cells at scale into the New Zealand health system.
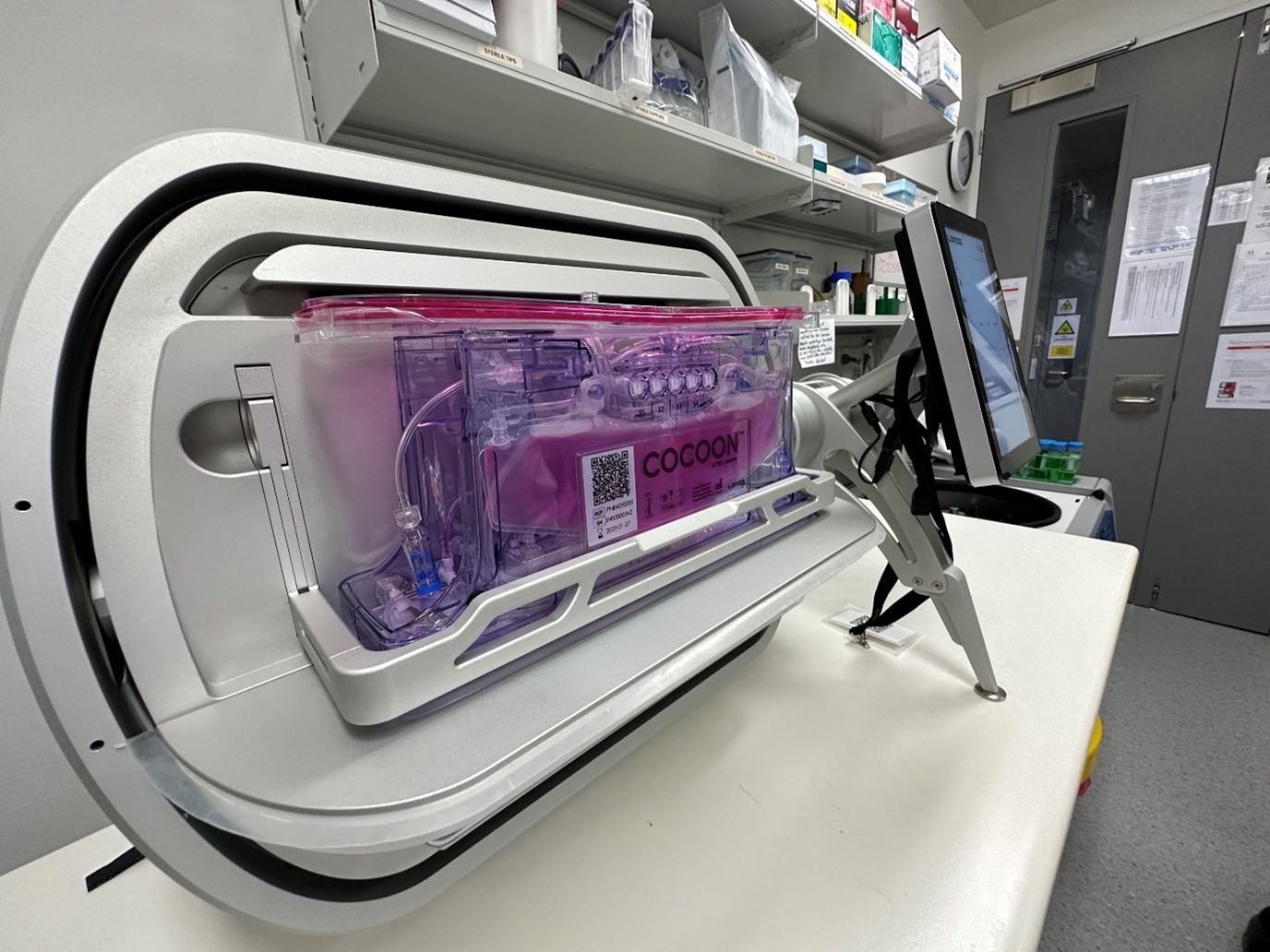
The process has been largely automated with manufacture of patient CAR T-cells taking place in a closed system – Lonza's Cocoon Cell Therapy Manufacturing Platform.
Leveraging the clinical wins
With the impressive safety profile of the treatment, the phase 1 trial transitioned to a dose expansion cohort and incorporated outpatient management, which is better for patients and their families, and a major cost-saving for the health service. The institute also started incorporating the new automated process for CAR T-cell manufacture with BioOra and gained regulatory approvals.
“The CAR T-cells made using the automated process are behaving just like the ones we used to make manually,” says Dr Weinkove.
“We’re seeing very similar product characteristics, very similar pharmacokinetics, and very similar safety and effectiveness outcomes. The new process is also providing higher CAR T-cell yields and saving on operator time.
“As a result, we’ve been able to embed this automation process as part of our manufacture going forward.”
Having treated a total of 30 patients through phase 1 and successfully validating and establishing the automated manufacturing process with BioOra, the Malaghan Institute now has the data and evidence to move to a larger phase 2 trial to confirm effectiveness and safety of the therapy.
Entering the next phase of clinical trials
The Malaghan Institute is aiming to treat an additional 60 patients with relapsed or refractory large B-cell lymphomas in their upcoming phase 2 trial. They’re optimistic that this might lead to the registration of the product in New Zealand and Australia.
BioOra, the fledgling CAR T-cell manufacturing company, is also spreading its wings heading into phase 2.
“We’ve gone from setting that capability up as a standalone company in 2021 to it now employing just short of 20 staff – and that growth trajectory is looking to continue,” Mr Zablocki says.
“The business is undertaking a separate capital raise and is setting itself up as a standalone commercial entity that can deliver Malaghan’s therapies and other cell therapies for New Zealand into the future.”
Bringing more clinical trials to New Zealand
The Malaghan Institute is keen to attract more clinical trials to New Zealand and confident that their trial has shown there are ways to make that happen.
“Through this programme, support has rallied around the opportunity that CAR T-cell therapy presents,” says Mr Zablocki.
“It’s come from Government with the likes of the MBIE Grant, it’s come from commercial avenues as well as the partnerships that we’ve attracted around this project, and there’s been huge philanthropic support for the programme in recognition of the urgent medical need.”
By harnessing those different areas of support, Mr Zablocki says that this programme has given New Zealand another model for delivering clinical trials that provide more options for people in need.
“Through this trial, we have been able to forge strong contacts with international leaders in the field of CAR T-cell therapies. We now aim to leverage this opportunity and create an even more ambitious programme that places New Zealand at the forefront of CAR T-cell development globally.”

More about the Malaghan Institute’s CAR T-cell programme(external link) — Malaghan Institute

